ALERT: Stay healthy this cold and flu season! Learn more
ALERTA: ¡Mantente sano durante esta temporada de influenza y resfriados! Más información
Date: May 18, 2023
Attention: All Providers
Master Provider File effective date: To Be Determined
Important provider notice: As a reminder, the Provider Enrollment and Management System (PEMS) is the required Texas Medicaid & Healthcare Partnership (TMHP) program which is the single tool for provider enrollment, reenrollment, revalidation, and maintenance requests (maintaining and updating provider enrollment record information) for Texas Medicaid. Clarifying information on PEMS can be found here: https://www.tmhp.com/news/2023-05-16-provider-enrollment-and-management-system-pems-post-deployment-update
Providers are strongly encouraged to visit this site for an overview of the most current PEMS information.
Some topics with clarifying information include the following:
As an MCO, TCHP will contract, credential and pay only those providers who are properly enrolled with TMHP and whose information is received in the official PEMS file from TMHP. In addition, it is important that every provider be enrolled at each location where they see patients. This is to help ensure claims process correctly.
UPDATE on guidance for practice location and license:
For your convenience we have included information on PEMS enrollment, provider requirements, and retro-active billing allowances at the end of this Provider Alert.
Resource: https://www.tmhp.com/topics/provider-enrollment
Resource: https://www.tmhp.com/news/2023-01-30-provider-enrollment-and-management-system-pems-post-deployment-update
How PEMS is accessed: PEMS is accessed through My Account. PEMS access is connected to the National Provider Identifier (NPI) or Atypical Provider Identifier (API) associated with the TMHP user account. Providers should ensure that the NPI has all the current and correct information. After a TMHP user account is created, follow these best practices for account management:
UPDATE on guidance for PEMS Enrollment Deficiencies: Providers have a total of 45 business days to complete and resolve all deficiencies when completing their enrollment application. PEMS will display the message “You must respond to and resolve all deficiencies within 45 business days.”
More information on provider enrollment identification:
More information on NPI:
More information on API:
Provider Requirements
Providers can view and confirm their revalidation date and enrollment information in PEMS here. As a reminder, effective May 11, 2023, the federal flexibility to extend Medicaid provider revalidation dates that were due during the federal COVID-19 PHE has ended.
UPDATE on guidance for revalidation dates: TMHP has sent an email to affected providers with a recalculated revalidation due date. Providers can find their revalidation due dates in the Provider
Dashboard in PEMS under the Revalidation Due Date field in the Enrollment Information section of the Provider Information page. To reduce application time, we encourage providers to have the following information available:
Providers revalidating an existing enrollment should continue to submit claims to meet their timely filing requirements. For provider enrollment help, click here.
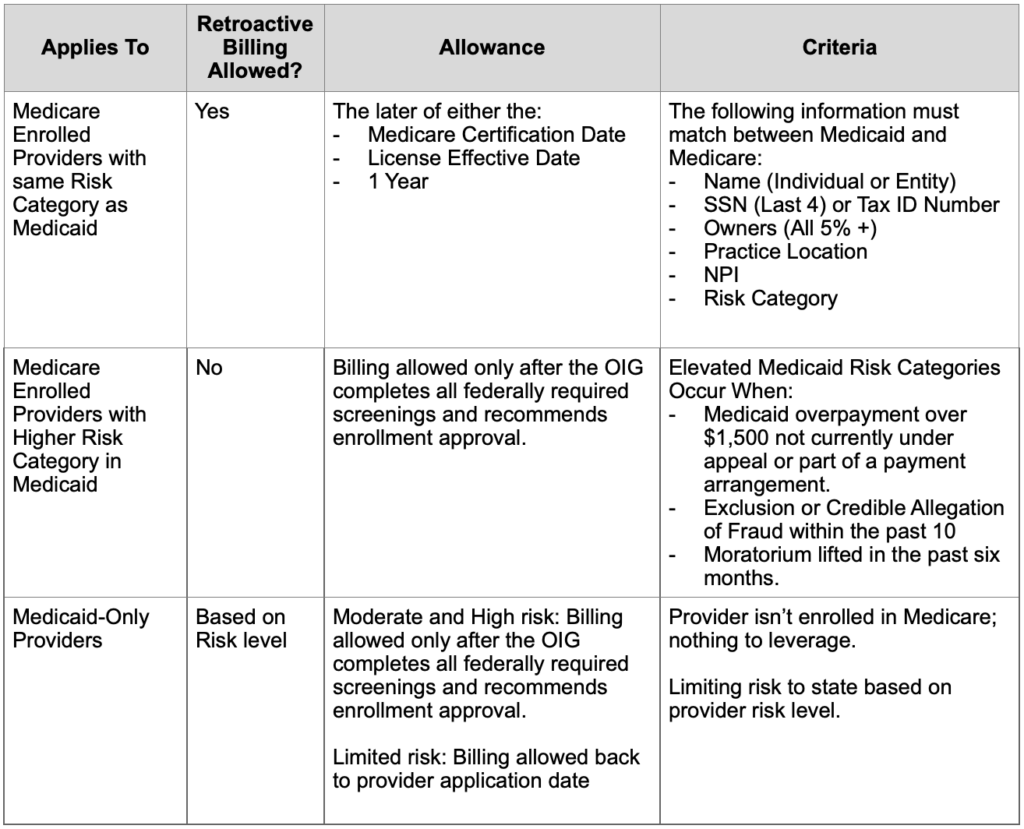
Provider effective dates: Prior to the PEMS implementation, the provider billing effective date could be the Medicare enrollment effective date, the provider license date, or the application completion date (retroactive billing date).
With PEMS implementation, new and reenrolled provider agreement effective dates were upon signature of the agreements and required all screenings to be completed. After further review, HHSC, in collaboration with the Office of Inspector General (OIG) made the decision to allow retrospective billing effective dates in certain circumstances, as outlined in the table below.
Retroactive Billing Allowances Table
If you have any questions, please email Provider Relations at: providerrelations@texaschildrens.org.
For access to all provider alerts, log into: www.thecheckup.org or www.texaschildrenshealthplan.org/for-providers.